476
Views & Citations10
Likes & Shares
Type 1 Diabetes Mellitus (T1D) arises from the autoimmune destruction of pancreatic beta cells responsible for insulin secretion. This results in severe endogenous insulin deficiency triggering hyperglycemia. An estimated 8.4 million people around the world had T1D in 2021. There were 23,096 TID cases in 2022 of which 27% were
Type 1 diabetes mellitus (TID) occurs as a result of the autoimmune destruction of pancreatic beta cells responsible for insulin production. The pathogenesis is thought to involve T cell mediated destruction of the beta cells. This results in severe endogenous insulin deficiency leading to hyperglycemia [1]. The definitive management for T1D is exogenous insulin therapy while its symptomatic onset is usually during childhood or adolescence but symptoms can develop much later. Therefore, a TID patient will often require life-long insulin treatment through insulin injections, an automated insulin delivery system or through the use of insulin pumps. The ideal regimen of insulin replacement maintains blood glucose in the normal physiological range while allowing flexibility in terms of mealtimes and activity levels. Without tight glucose control, the patients run the risk of developing life-threatening complications such as diabetic ketoacidosis in addition to other microvascular and macrovascular complications [2]. An estimated 8.4 million people around the world had T1D in 2021, and this number may rise to 17.4 million by 2040 [3]. 21% of T1D cases live in Low and Low-Middle Income Countries while Sub-Saharan Africa accounts for 4% of the global prevalence and 23% of lives lost each year [3]. In 2022, a total of 530,000 new cases of T1D were reported worldwide [4] cutting across all ages, of which 38% were
Under the theme “Diabetes is a family affair”, WHO stress the need for familial psychosocial support to enable the child to take insulin as advised, monitor blood sugar daily and keenly partake healthy diet [6]. Parents are encouraged to consult with schools and other institutions attended by the child for synergistic physical and psychological backup [6]. This support encourages adherence to insulin uptake, consistent follow-up visits and healthy living. Inadequate patient education can lead to poorly controlled sugars hence higher risk of complications [6]. This emphasizes the need to strengthen patient education for better health outcomes.
The African Region under the article “No-Cost Diabetes Care Saving Young Lives in Kenya” observed that many children living with T1D that require daily insulin to survive died before diagnosis [7]. Inadequate care was noted as a great impediment in controlling T1D after diagnosis. With most children coming from poor families which cannot afford insulin, glucose strips, glucometers, needles and hospital consultation, such programs are deemed game changers in the management of T1D in children [7]. In Gabon, the factors linked to poor outcomes included the high cost of treatment and the insufficiency of patient therapeutic education.
Glucose Control and Adherence
During glucose control, typical regimens constitute basal insulin to restrain gluconeogenesis and ketogenesis in the pre-prandial state, mealtime insulin to cover the intake of carbohydrates and other macronutrients; and correction insulin to manage hyperglycemia [9]. Despite advances in technology that ease insulin delivery with pens or pumps, adherence to anti-diabetics regimens is often problematic for patients of all ages, but most difficult for adolescents [10]. This complexity in insulin use and dietary intake is challenging for adolescents. In addition, adherence is further complicated by the discomfort of painful needle sticks required for blood glucose monitoring and the inconvenience of carrying or wearing insulin administration devices. Therefore, mean HbA1c levels are averagely higher than the recommended 7.5% in most countries ranging from a low of 17% of adolescents meeting the target in Wales to 49% of such adolescents in Sweden [11]. This is similarly the case in Kenya.
Teens have difficulty achieving and maintaining target glycemic control as a number of factors converge. Additionally, adherence is likely to grow more difficult as providers intensify regimens to improve glycemic control for better outcomes with the inadvertent result of increasing burden and reducing health-promoting behavior [12,13]. Interventions to improve adherence in this group may include family-based therapies, motivational interviewing and technology-based applications among others [14]. Provider communication is key in facilitating adherence behaviors in adolescents with T1D. Interventions that focused on direct behavioral processes and neglected emotional, social and family processes were unlikely to have an impact on glucose control [15]. Multicomponent interventions showed more robust effects on HbA1c [15]. Keeping more appointments and taking diabetes medications as directed were associated with substantial improvements in Hb1Ac. This study illustrates the impact of a package incorporating facility-based adherence counselling and motivation approaches in enhancing adherence to T1D treatment among children and adolescents.
Study Aim
This study sought to evaluate whether facility-based health education, adherence counselling, and motivation can significantly improve blood glucose control based on routine HbA1c values among T1D clients in Vihiga County, Kenya.
METHODS AND METHODOLOGY
Intervention Package
The intervention targeted T1D patients in Vihiga County enrolled for continuous care at Vihiga County Referral Hospital. The referral hospital is the primary, Level 4 public county government referral hospital with the capacity to diagnose and treat T1D patients. Facility-based health education was provided to clients in three sessions three months apart. The health education was individualized to the needs of each patient but with a focus on adherence to insulin and healthy dietary options. During the study period, 25 T1D patients received 2 home visits each. Challenges that were brought up by the clients were addressed through health education and health promotion. There were also two sessions of motivation held outside the clinic setting. Due to the risk of microvascular complications, the clients were all provided closed shoes, referred to as ‘crocks. Females also received menstrual pads during the visit as a form of extrinsic motivation. Health talks and motivational speeches were also provided by various health professionals including one ambassador of T1D. During routine quarterly visits to the hospital, HbA1c values were evaluated and documented which formed the basis of the comparative findings of this study.
Study Design, Setting, Sample and Data analysis
This study used a mixed method study employing both qualitative and quantitative study design. Quantitative study used a retrospective Cross-sectional study framework where paired sample records were reviewed, while the qualitative study design utilized a descriptive and interpretive Phenomenology methodology. The latter was deemed important since the researchers did not assume they were completely clueless about the issues related to managing T1D patients [16]. The intervention targeted T1D patients in Vihiga County Referral Hospital. The hospital is classified as a Level 4 hospital where most of the specialized services are offered in the County. Records of T1D patients who had had at least three appointment visits with documented random blood sugars (RBS) and HbA1c values were evaluated and HbA1c values extracted.
The study employed purposive sampling by targeting records of all T1D patients reviewed at Vihiga County Referral Hospital between the period of July 2022 to Jan 2023. 32 patient records were identified. Due to the lack of cartridges for HbA1c immunoassays, and financial limitations associated with procuring the testing services in the County referral hospital, only two sessions of HbA1c testing were done in July 2022 and January 2023.
Data analysis was done using STATA/BE 17.0 for quantitative data. The student’s t-test was used to statistically determine changes in HbA1c values between July 22 and January 2023. Spearman correlation was applied to establish the relationship between age and HbA1c values. Qualitative data was analyzed through thematic analysis by two different researchers to arrive at the final themes. This was an operational research whose ethical approval is covered by the umbrella protocol approval number ERC 31/6/22-07, approved by the Ethics and Research Committee at the Jaramogi Oginga Odinga University of Science and Technology (JOOUST). The patient records were anonymized through de-identification to protect their identity.
RESULTS
Quantitative Results
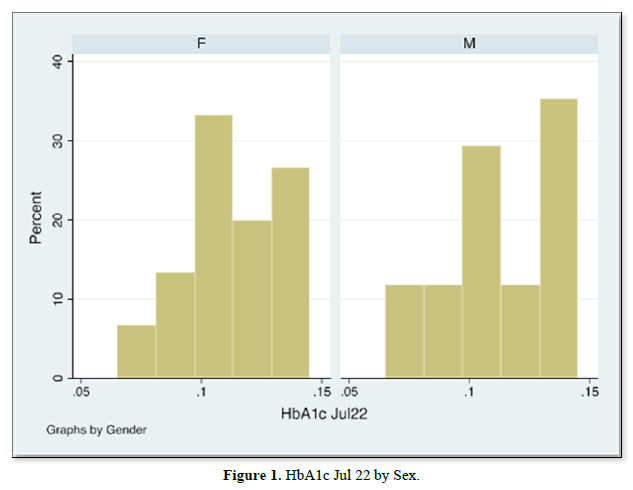
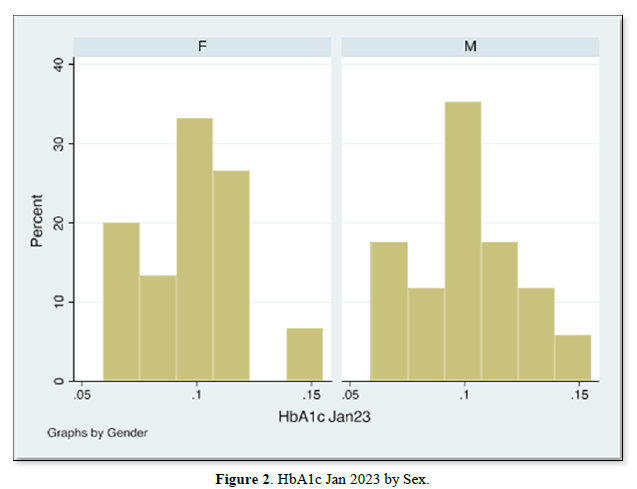
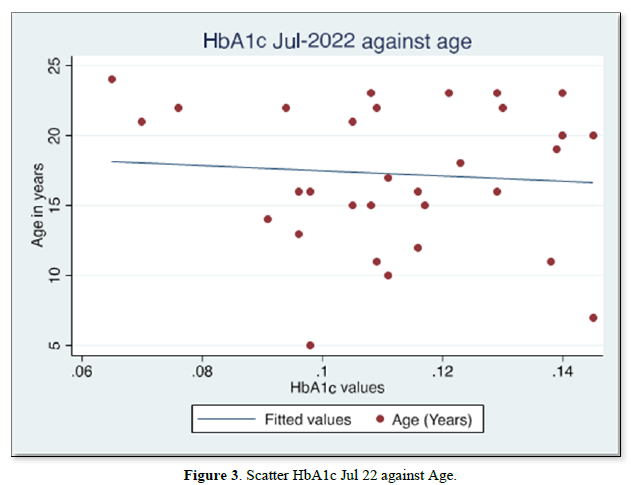
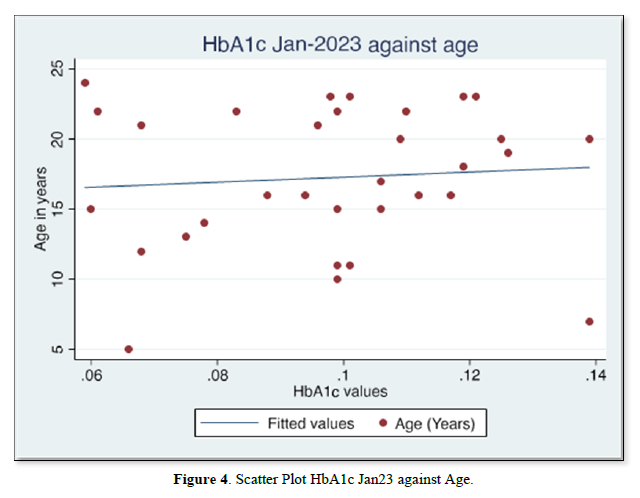
The results of gender distribution, age of participants, mean HbA1c values are shown in (Table 1) below. Similarly, Figures 1 & 2 below illustrate histograms showing the gender- categorized HbA1c values for July 2022 and January 2023. The scatter plots in Figures 3 & 4 depict the relationship between HbA1c and age as per July 2022 and Jan 2023 findings.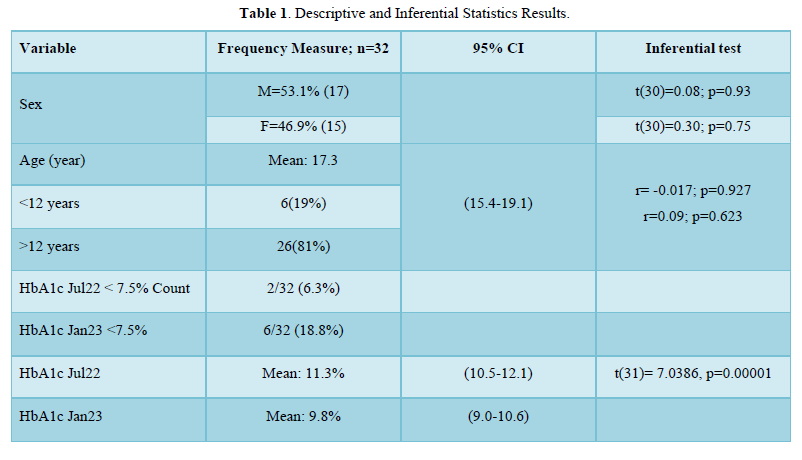
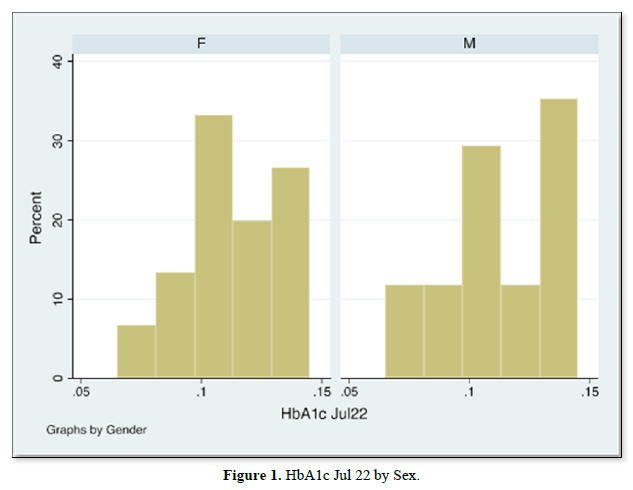
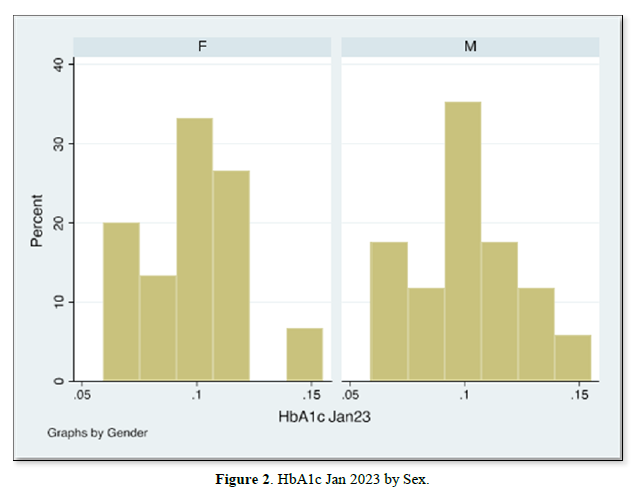
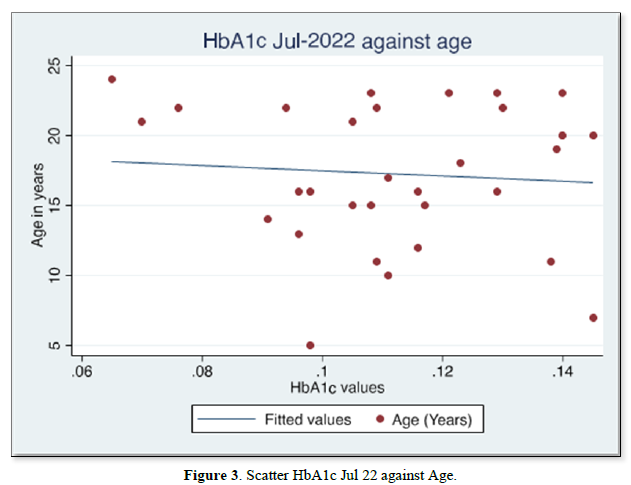
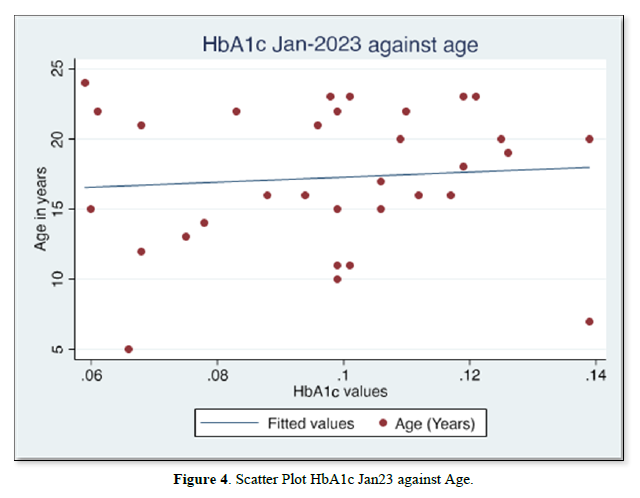
The results also showed that HbA1c levels as assessed in July 2022 did not statistically differ based on Sex [t-test t(30)=0.08, p=0.93]. Similarly, the difference in Jan 2023 HbA1c levels between sexes was not significant [t-test t(30)=0.30, p=0.75]. Although there were changes in values of HbA1c with age for both July 2022 and Jan 2023 HbA1c values, age did not significantly correlate with either July 22 values [r= -0.017, (p=0.927, n=32)], nor Jan 23 values [r=0.09, (p=0.623, n=32)]. There was equally no notable significant correlation between period- since diagnosis and HbA1c levels July 22 [(r=0.06, (p=0.75, n=32)], nor Jan 23 [r=0.75, (p=0.623, n=32)]. A multivariate analysis showed that there was no significant association between glycemic control in Jan 23 and period since diagnosis (p=0.18), nor age (p=0.28).
Qualitative Findings
23 participants were asked whether they would recommend the hospital-based services and the motivation package to another person or client. 22 participants responded “Yes” to the question. They were also asked to explain why they would or would not recommend the package of service to a different client in addition to challenges they may experience related to the management of their T1D. The reasons given were clustered into themes as indicated below.
Positive reasons for recommending services
Friendly and Dedicated team at the facility. “Polite” “friendly health service provider” “reminders for revisit dates” “Calls by health service provider to check on patients” “Staff understand and care for diabetic patients”.
Good Services “very comfortable with services received” “fast Services” “Good services” “availability of tests and drugs prescribed”
Reasons for not recommending services
“Long queues” “Delay in Services at the facility” “Late start of clinics at times”
Challenges experienced when using insulin at home
Injection discomfort/adverse drug reaction
“Pain at injection site” “swelling at injection” “feeling tired after injection
Low blood glucose
“Anxiety when sugar levels go down” “Sometimes not sure if still to inject with insulin when glucose levels are low” “Low glucose levels at times”
Economic barriers
“No food at home” “many thoughts due to lack of income” “poor feeding” “No glucometer to self-monitor”
Insulin storage challenges
“Failure to work due to poor storage” “difficult storage”
Insulin stock-out
“insulin doses not enough” “shortage of insulin at times” “sometimes insulin is out of stock”
DISCUSSION
The mean age of the participants was 17 years. The percentage of patients with controlled blood glucose through their HbA1c values was only 2 (6.3%) in July 2022 compared to 6 (18%) in January 2023 as shown in table 1. The percentage of patients with controlled blood glucose is lower than what has been reported in a study done to assess the prevalence of well-controlled blood glucose for TID in Kenya [17]. However, the latter study had more children among the participants, 21(78%) than adolescents arriving at the conclusion that younger children tend to exhibit better glycemic control compared to older children and adolescents [17]. This study, however, did not find any correlation between age and HbA1c levels in contrast to other studies [17,18]. The study by Djonous [18] only had 10(10.5%) participants aged below 12 years compared to 6(18%) in this study. A study done in Tanzania, though more than a decade ago, showed only 1% of children had good glycemic control [19].
In this study, there was a notable improvement in mean HbA1c levels as measured between the two periods from 11.3% in July 2022 to 9.8% in January 2023. Although the mean HbA1c values were still higher than the 7.5% recommended target, there was a statistically significant improvement from the mean values reported in July 2022. This could be attributed to the intervention package delivered. The package consisted of provider-directed adherence counselling targeting adolescents and their parents. Contingency management through providing the clients with shoes dubbed “crocks” and sanitary pads for females was also offered twice between July 2022 and January 2023. Incentives are argued, through some studies, to be a positive reinforcement towards adherence to glucose monitoring among adolescents [20]. However, Wong’s [20] study did not find financial incentives as having a significant impact on glycemic control in contrast to the findings of this study. Nevertheless, motivational interviewing, parent-directed and hospital-based contingency management aimed at enhancing the monitoring of blood glucose equally significantly improved HbA1c levels [21]. This suggests that a multicomponent intervention package consisting of adherence emphasis and extrinsic motivation through gifts could enhance adherence to TID self-management and help improve HbA1c levels as suggested through this study’s findings. In addition, there is a need to consider supporting the clients to acquire continuous glucose monitoring options, and automated insulin delivery systems to enhance glucose control.
From the qualitative findings, 22(96%) of the TID patients would recommend the diabetic-related management services offered at the hospital to others. The positive attributes associated with the services include the staff that were commonly described as friendly and dedicated. This attribute was linked to the staff’s effort in ensuring that the patients are reminded to attend their clinics timely, friendly demeanour and call to check on patients on non-clinic days. The services were acceptable to the patients as they were generally described as “good”. Despite most patients giving positive comments as to why they would recommend the services to another client, there were some who gave both positive and negative attributes. The latter includes longer waiting times during clinic days, especially quarterly clinic days. The quarterly clinic days in the hospital are synchronized for the children and adolescents to allow the cohort to meet and share, in a similar approach to psychosocial support groups [22]. Challenges identified by the participants include insulin injection-related adverse drug reaction (ADR), hypoglycemia, economic barriers that limit routine glucose monitoring, HbA1c assessment, interrupted insulin availability, food shortage and difficulties in the storage of insulin. Apart from the ADR-related challenges, the others have socioeconomic origins. Even though insulin is often provided for free to T1D clients in the county, through the CDiC (Changing Diabetes in Children) program primarily run by Novo Nordisk, occasional stockouts of the product necessitating contingency measures to avail the product do occur. Nevertheless, no client went without insulin between July 2022 and Jan 2023. Similarly, the HbA1c immunoassay testing machine and its corresponding cartridges are provided and replenished through the support of CDiC allowing the service to be offered for free to the clients. However, a prolonged stock out of the item meant that the November 2022 quarterly HbA1c assessments could not be done. Regarding the storage challenge, a participant mentioned that they feared insulin failure due to poor storage “Failure to work due to poor storage”. It is possible that a study participant would not find a suitable place in their places of abode that can maintain room temperature throughout the course of insulin storage. This is something that requires further exploration to ascertain the exact challenges experienced at home linked to insulin storage since it hugely depends on the home/house environment. One client also reported emotional distress captured as “feeling low”, in the course of self-management. Psychological issues are notable concerns among some diabetic patients as reported through various research in Africa and beyond [23,24]. In Zambia, such adolescents had adopted acceptance and avoidance as possible coping strategies [24]. Nevertheless, this informs the need for mental health professionals as part of the core team in the management of TID [25]. Concerns also emerged regarding low glucose levels or potential low glucose levels among some patients. Not all TID patients are able to self-monitor their glucose levels due to insufficient glucometers. Some glucometers had been provided earlier to the patients but they were insufficient to meet the needs of newer patients. Due to financial challenges and the poor socioeconomic background associated with most TID patients, they were unable to purchase their glucometers and had to rely on donated batches. Nevertheless, the uncertainty on whether to self-administer insulin or not when suspecting hypoglycemia implies that the patients further require individualized health education and counselling on when to administer insulin and requisite dose adjustments based on blood glucose levels and dietary intake.
STUDY LIMITATIONS
The study was limited by the number of study participants, 32 compared to higher numbers reported through other studies. In addition, the qualitative findings may not be transferrable due to the subjectivism of the methodology. Although key in triangulating data, respondent validation was not employed hence the researchers did not have an opportunity to ascertain the qualitative responses from the participants.
CONCLUSION
The multicomponent intervention package prioritizing adherence counselling and extrinsic motivation can be resourceful in improving glucose control outcomes among TID patients. However, there is a need for more support to enable the patients to acquire more advanced glucose control options that allow the recognition of abnormal blood glucose levels necessitating timely control. This includes options such as Continuous Glucose Monitoring (CGM), insulin pumps and automated insulin delivery systems to enhance tight control of blood glucose and better quality of life.
- Lu X, Zhao C (2020) Exercise and Type 1 Adv Exp Med Biol 1228: 107-121.
- Ehrmann D, Kulzer B, Roos T, Haak T, Al-Khatib M, et al. (2020) Risk factors and prevention strategies for diabetic ketoacidosis in people with established type 1 Lancet Diabetes Endocrinol 8(5): 436-446.
- Gregory GA, Robinson TIG, Linklater SE, Wang F, Colagiuri S, et al. (2022) Global incidence, prevalence, and mortality of type 1 diabetes in 2021 with projection to 2040: A modelling study. Lancet Diabetes Endocrinol 10(10): 741-760
- International Diabetes Federation Atlas (2022) Reports. Available online at: https://diabetesatlas.org/2022- reports/International
- Katte JC, McDonald TJ, Sobngwi E, Jones AG (2023) The phenotype of type 1 diabetes in sub-Saharan Africa. Front. Public Health 11: 1014626.
- World Health Organization (2019) World Diabetes Day 2019-Message of WHO Regional Director for Africa, Dr Matshidiso
- World Health Organization Africa (2021) No-cost diabetes care saving young lives in
- Damiens AP, Zandzou PSG, Ibounde ET, Kay's SK, Baye E, et al. (2019) Type 1 diabetes mellitus in Gabon: A study of epidemiological aspects. Int J Pediatr Adolesc Med 6(3): 87-91
- Holt RIG, DeVries JH, Fischl AH, Hirsch IB, Kirkman MS, et al. (2021) The Management of Type 1 Diabetes in Adults. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 44 (11): 2589-2625.
- Borus JS, Laffel L (2010) Adherence challenges in the management of type 1 diabetes in adolescents: prevention and intervention. Curr Opin Pediatr 22(4): 405-411.
- Charalampopoulos D, Hermann JM, Svensson J (2020) Improving clinical outcomes in newly diagnosed pediatric Type 1 diabetes: Teamwork, targets, technology, and tight control-The 4T Front Endocrinol 11: 360.
- Svoren BM, Volkening LK, Butler DA, Moreland EC, Anderson BJ, et al. (2007) Temporal trends in the treatment of pediatric type 1 diabetes and impact on acute J Pediatr 150: 279-285.
- Silverstein J, Klingensmith G, Copeland K, Plotnick L, Kaufman F, et (2005) Care of children and adolescents with type 1 diabetes: A statement of the American Diabetes Association. Diabetes Care 28: 186-212.
- Datye KA, Moore DJ, Russell WE, Jaser SS (2015) A Review of Adolescent Adherence in Type 1 Diabetes and the Untapped Potential of Diabetes Providers to Improve Curr Diab Rep 15(8): 51.
- Hood KK, Rohan JM, Peterson CM, Drotar D (2010) Interventions with Adherence-Promoting Components in Pediatric Type 1 Diabetes: Meta-analysis of their impact on glycemic Diabetes Care 33(7): 1658-1664.
- Matua GA, Der Wal DM (2015) Differentiating between descriptive and interpretive phenomenological research Nurse Res 22(6): 22-27.
- Ngwiri T, Were F, Predieri B, Ngugi P, Lorenzo I (2015) Glycemic control in Kenyan children and adolescents with Type 1 Diabetes Int J Endocrinol 2015: 1-7.
- Djonou C, Tankeu A, Dehayem M, Tcheutchoua D, Mbanya J, et al. (2019) Glycemic control and correlates in a group of sub Saharan type 1 diabetes BMC Res Notes 12(50): 1-5.
- Majaliwa E, Munubhi E, Ramaiya K, Mpembeni R, Sanyiwa A, et al. (2007) Survey on Acute and Chronic Complications in Children and Adolescents with Type 1 Diabetes at Muhimbili National Hospital in Dar es Salaam, Diabetes Care 30(9): 2187-2192.
- Wong CA, Miller V, Murphy K, Small D, Ford C, et al. (2017) Effect of Financial Incentives on Glucose Monitoring Adherence and Glycemic Control Among Adolescents and Young Adults with Type 1 Diabetes. JAMA Pediatr 171(12): 1176-1183.
- Stanger C, Ryan S, Delhey L, Thraikill K, Zhongze Li, et al. (2013) A Multicomponent Motivational Intervention to improve adherence Among adolescents with poorly controlled Type 1 Diabetes: A Pilot J Pediatr Psychol 38(6): 629-637.
- Delamater A (2009) Psychological care of children and adolescents with Pediatr Diabetes 10(Suppl. 12), 175-184.
- Gonzalez J, Tanebaum M, Commissariat P (2016) Psychosocial factors in medication adherence and diabetes self-management. Implications for research and Am Psychol 71(7): 539-551.
- Hapunda G, Abubakar A, Vijver F, Pouwer F (2015) Living with type 1 diabetes is challenging for Zambian adolescents: qualitative data on stress, coping with stress and quality of care and BMC Endocr Disord 15(20): 1-7.
- Kaira S, Naraya B, Yeravdekar R (2018). Emotional and psychological needs of people with diabetes. Indian J Endocrinol Metabol 22(5): 696-704.